Researchers at The Wistar Institute have engineered a novel DNA vaccine to target a group of proteins that are particularly overexpressed in various cancers. The new vaccine, focusing on the human cancer-associated MAGE-A group of proteins, has been successfully tested and is safe in melanoma preclinical model. The study has been published online in Clinical Cancer Research.
This new methodology can disentangle immunotherapy treatment and may avert cancer escape from immune pressure as the immune framework could assault cancer at different susceptible targets. Proteins belonging to the MAGE-A family represent potential targets for immunotherapy as their expression is limited to cancer cells. However, cancer vaccines targeting the original MAGE-A3 member, have the maximum expression in several solid tumors and have up to this point neglected to exhibit viability in clinical preliminaries.
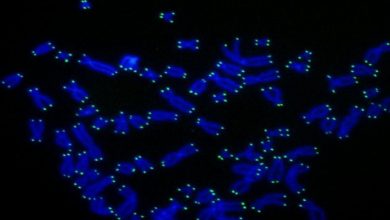
Scientists at Wistar conducted a systematic examination of the expression levels of all the twelve proteins in the MAGE-A family in human cancers to resolve this problem and advance the clinical applications of this promising immunotherapy. They saw that huge numbers of the MAGE-A members, and not simply MAGE-A3, are very communicated on tumor cells in a few growths composes, some of them being available at the same time in a similar patient. These discoveries propose that past immunizations with a constrained spotlight on one target were likely not compelling in driving solid T-cell resistance as a result of the characteristic immune hosing framework known as immune tolerance.
“The combination of structural design and synthetic DNA technology offers ample flexibility and specificity in the development of a designer target immunogen,” said lead researcher David B. Weiner, Ph.D., executive vice president of The Wistar Institute, director of The Wistar Institute Vaccine & Immunotherapy Center, and W.W. Smith Charitable Trust Professor in Cancer Research. “We amalgamated structurally relevant primary sequences from multiple MAGE-A members, obtaining an optimized consensus DNA vaccine capable of targeting seven MAGE-A family members simultaneously. This vaccine is recognized by the host immune system much more robustly, resulting in improved immune performance.”
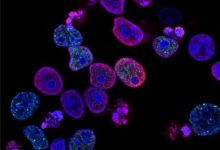
Tried in mice, the vaccine initiated safe cross-response with various MAGE-A proteins and instigated a strong CD8+ T cell-intervened immune reaction.
“CD8+ T cells are the predominant effectors in the response to immunotherapy; we can think of them as the Navy Seals of cancer immunology,” added Weiner.
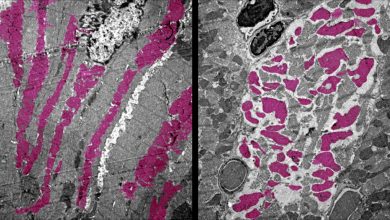
Imperatively, the immunization altogether impeded tumor development and delayed survival in a mouse model of melanoma. The specialists watched lessened intrusion in the skin, which was related with aggregation of CD8+ T cells into the tumors, showing the capacity of the immunization to drive antitumor resistance of significance for melanoma treatment.
“Our cross-reactive vaccine has a significant advantage in preventing tumor escape compared to previously designed MAGE-A3-specific vaccines,” said Elizabeth K. Duperret, Ph.D., a postdoctoral fellow in the Weiner Lab and first author on the study. “Patients whose tumors express multiple members of this family of antigens represent an important group to study the benefits of this immunotherapy approach.”