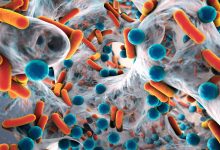
In a leading research conducted at the Research Institute of McGill University Health Centre (RI-MUHC), the scientists have identified new means of fighting drug-tolerant bacteria, which has become a growing global threat. It is considered as dangerous as the drug-resistant microbes. Till date, there is not much information available about the mechanisms that lead to tolerance. Tolerance is a strategy that makes bacteria “indifferent” to antibiotics and almost “un-killable,” which results in chronic infections extremely difficult to treat and cure.
The study was conducted on Pseudomonas aeruginosa, that has been listed among the “nightmare bacteria” by the Centers for Disease Control and Prevention (CDC) in the United States, with an estimated 51,000 healthcare-associated infections each year resulting in around 400 deaths. It is also a common cause of healthcare-associated infections such as pneumonia, bloodstream or urinary tract infections, and surgical site infections.
The bacterium has the tendency of becoming highly tolerant to the antibiotics. “P. aeruginosa causes lifelong lung infections in individuals with cystic fibrosis, and these infections cannot be cleared, even by cocktails of the most potent antibiotics available,” says Dr. Nguyen, who is also a respirologist at the MUHC.
In the new research, Dr. Nguyen and her team were able to identify a new function which plays an important role in antibiotic tolerance and it could be targeted to enhance the currently available antibiotics. “Many bacteria, such as P. aeruginosa, when they grow slowly or do not grow at all, become tolerant to antibiotics,” explains first study author Dorival Martins, a senior post-doctoral fellow in Dr. Nguyen’s laboratory. This is a crucial problem because the majority of the chronic infections are caused by slow-growing bacteria that enters into a dormant state inside the living host.
The researchers have discovered that when P. aeruginosa is under stress or lacking nutrients, it uses a stress signaling system and defense enzyme (superoxide dismutase) to modify its cell membrane, making it less permeable to molecules and preventing antibiotics from penetrating the cell. So, if the enzyme activity or the stress signaling system could be inhibited then it can render the bacteria more susceptible to the antibiotics.
Up until now, the antibiotic tolerance in slow-growing the pathogen was majorly linked to the fact that targets of the antibiotics were not available in dormant cells. But now with this research scientists have been able to establish a link between the stress signaling system, defense enzyme and antibiotic tolerance. This could expand the utility of our antibiotics and make new ones more effective.